Dental Appliances for Sleep Apnea: Pros and Cons
Although continuous positive airway (CPAP) pressure therapy is the most recommended treatment for patients with obstructive sleep apnea (OSA), not all patients are able to remain compliant with this form of treatment. Some complain of claustrophobia, dry nasal passages, skin irritation from masks, difficulty tolerating pressurized air, and accidentally removing the mask while tossing at night.
For patients like these, an alternative to CPAP therapy may be recommended, and depending on the level of severity of their disorder, may benefit from a substitute treatment such as an oral dental appliance.
What is an Oral Dental Appliance for Sleep Apnea?
Before diving into how oral appliances work, lets have a brief recap on what sleep apnea is, and how it affects your sleep and health. [If you’re already familiar with how sleep apnea works, scroll down to dental appliances]
Obstructive Sleep Apnea
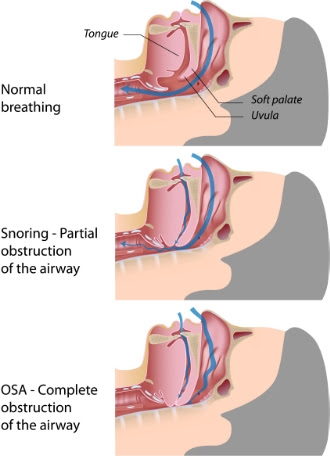
Obstructive sleep apnea is a sleep disorder in which a person stops breathing periodically throughout the night due to physical obstructions of the airway. These stops in breathing usually last for around ten seconds and are often followed by snorts, gasps, or choking sounds as a person’s body fights to resume breathing again.
When you sleep, the muscles in your body relax so they can begin to repair themselves to keep you healthy and active everyday. However, muscles in your mouth and throat also relax during sleep, and for some people (an estimated 18-20 million U.S. adults) these muscles along with soft fatty tissues relax to the point where they fall back into the upper airway and block the flow of oxygen from coming in.
When you stop breathing during the night, your brain responds by partially waking to send signals to the respiratory system to work harder to get past the obstruction.
Side effects of obstructive sleep apnea include
- high blood pressure
- heart arrhythmias
- heart disease
- heart attack
- stroke
- increased risk of diabetes
- and even death
Sleep apnea even leads to excessive daytime sleepiness because each time your brain has to “wake up” to tell your body to continue breathing, it’s not spending enough time doing all of the other functions that are necessary of quality sleep. Being tired all day can cause poor performance at work or school, memory and other cognitive troubles, depression, and even accidents while driving or while at work.
How severe one’s sleep apnea is can be determined by the amount of apnea events (pauses in breathing):
Mild OSA: The sufferer experiences 5-14 episodes of interruptions in breathing in an hour.
Moderate OSA: The sufferer experiences 15-30 episodes of interruptions in breathing in an hour.
Severe OSA: The sufferer experiences 30 or more interruptions in breathing in an hour.
Dental Appliances for sleep apnea
Before any treatment options can be determined, a sleep study must first be performed to determine the severity of one’s symptoms as it can have a direct influence on the recommended therapy.
The most common form of therapy is continuous positive airway pressure (CPAP) devices, which blow a steady stream of pressurized air through a mask into the respiratory system. For moderate to severe sleep apnea patients, most sleep professionals will recommend CPAP therapy as a first-line treatment option.
For mild to moderate sleep apnea, a dental device is often the recommended therapy. Dental devices may also be recommended to be worn in conjunction a CPAP device to help lower high pressure needs.
How do dental appliances work?
There are two major categories of dental devices:
- Mandibular advancement devices (MADs)
- Tongue Retaining Mouthpieces
MADs used to treat sleep apnea look very similar to sports mouthguards or orthodontic retainers. They fit into the mouth by snapping over the upper and lower dental arches and have metal hinges connecting the two pieces: one fits over the upper teeth, and the other fits over the lower teeth.
MADs work by pushing the lower jaw and tongue slightly forward, which helps prevent throat muscles and issues (such as the pharynx) from collapsing back into the airways allowing for normal breathing during sleep. Most MADs are adjustable, allowing for dentists to fine-tune the position of the jaw for maximum effectiveness.
Tongue retaining mouthpieces are similar in construction to the MAD, but has a small compartment that fits around the tongue using suction to keep it held forward, preventing it from collapsing back into the airway. These devices are mostly used in patients who cannot adequately have their jaw repositioned forward.
Getting dental devices
You will have to have your dentist make a custom fitted oral device to suit your particular needs. Over-the-counter options are available, but not recommended. Over-the-counter devices may be appealing because of their reduced prices, but can actually complicate sleep apnea. Many patients who order oral devices without consulting with a dentist, find that their snoring symptoms went away, but were unaware that it was not preventing apnea events leading to complications down the road as only the snoring symptom was prevented but the disorder itself was not.
Pros of Dental devices
- Many patients find dental devices to be more comfortable and tolerable to wear as opposed to CPAP masks.
- Patients on CPAP often complain of dry, itchy noses from the air pressure drying out their sinuses. Oral devices do not have this problem.
- There is less equipment to become entangled with during sleep, or knock off during slumber, for patients who are active movers during sleep.
- There is a lot less equipment involved, and therefore easier to travel with.
Cons of Dental devices
- Jaw pain, soreness, or tension
- Sore teeth and/or gums
- Excessive salivation or even dry mouth
- Possible damage or permanent change to jaw position/bite
- Loosening of dental restorations (crowns, bridges, etc)
Who qualifies for dental appliances?
- Patients with mild to moderate sleep apnea (not recommended for moderate to severe sleep apnea)
- Patients with primary snoring (in absense of sleep apnea)
- Patients who have tried and failed at CPAP therapy may qualify
- Patients who were unsuccessful with or refused surgeries such as tonsillectomy, adenoidectomy, cranofacial operations, or tracheostomy.
- In combination with CPAP device to help lower patient’s apnea/hypopnea index for more tolerable air pressure settings.
If you’re concerned you have sleep apnea you should contact your local sleep clinic to schedule a consultation with a sleep specialist or talk with your primary care physician about your sleep troubles. Be sure to ask them about all of the available treatment options including CPAP and dental devices and inquire which may be best suited for you.